What might go wrong?
As with all major surgical procedures, complications can occur. This document doesn't provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following revision arthroplasty of the hip include:
- anesthesia complications
- thrombophlebitis
- infection
- dislocation
- myositis ossificans
- loosening
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but it is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection can be a very serious complication following an artificial joint revision. Some infections may show up very early, even before you leave the hospital. Others may not become apparent for months, or even years, after the operation. Infection can spread into the artificial joint from other infected areas. Your surgeon may want to make sure that you take antibiotics when you have dental work or surgical procedures on your bladder and colon to reduce the risk of spreading germs to the joint.
The risk of infection is higher in revision joint replacement than in primary joint replacement. In a primary hip replacement, the risk of infection is 0.5 to one percent. It goes up to two percent or more in revision cases. These figures are only an estimate and vary between different scientific studies.
Dislocation
Just like your real hip, the revised artificial hip can dislocate if the ball comes out of the socket. There is a greater risk just after surgery, before the tissues have healed around the new joint, but there is always a risk. A physiotherapist will instruct you very carefully on how to avoid activities and positions that may have a tendency to cause a hip dislocation.
Myositis Ossificans
Myositis ossificans is a curious problem that can affect the hip after both a primary hip replacement and a revision hip replacement. The condition occurs when the soft tissue around the hip joint begins to develop calcium deposits. Myositis means inflammation of muscle and ossificans refers to the formation of bone. This can lead to a situation where bone actually forms completely around the hip joint. This leads to stiffness in the hip resulting in much less motion in the hip joint than normal. It also causes pain.
Myositis ossificans is more common in people who have a long history of osteoarthritis with multiple bones spurs. Something about the genetic makeup in these people makes them more likely to produce bone tissue. Major reconstruction operations such as a hip revision seem to do more damage to the surrounding tissues than primary hip replacements. The operation is simply longer and harder to do. Calcium deposits are also more likely to form.
The treatment of myositis ossificans may actually begin before you get it. In cases where you are at high risk for developing this condition, your surgeon may recommend that you take medications such as indomethacin after surgery. This medication reduces the tendency for bone to form and may protect you from developing myositis ossificans.
A much more effective method that has been used a great deal to prevent the development of myositis ossificans involves radiation treatments immediately after surgery. These are the same type of radiation treatments used to treat cancer. Several short radiation treatments begun the day after surgery and continued for three to five days seem to drastically reduce the risk of developing myositis ossificans.
If myositis ossificans forms despite these precautions, treatment will depend on how much it affects your hip--how much pain it causes and how much it restricts motion. In some severe cases, you may choose to have a second operation to remove the calcified tissue that has formed. This is usually followed by radiation treatments to prevent the calcium deposits from returning.
Loosening
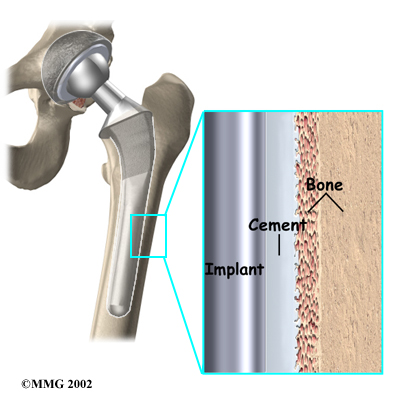
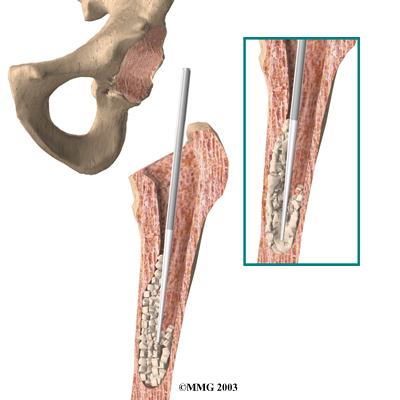
The major reason that artificial joints eventually fail continues to be a process of loosening where the metal or cement meets the bone. A loose revised prosthesis is a problem because it causes pain. Once the pain becomes unbearable, another revision surgery may be needed. The rate of loosening of revision arthroplasties is higher than in primary arthroplasties.
After Surgery
What happens after surgery?
After surgery, your hip is covered with a padded dressing. Special boots or stockings are placed on your feet to help prevent blood clots from forming. A triangle-shaped cushion may be positioned between your legs to keep your legs from crossing or rolling in.
If your surgeon used a general anesthesia, a nurse or respiratory therapist will visit your room to guide you in a series of breathing exercises. You'll use an incentive spirometer to improve breathing and avoid possible problems with pneumonia.
Physiotherapy treatments are scheduled one to three times each day as long as you remain in the hospital. Your first treatment is scheduled soon after you wake up from surgery. Your therapist will begin by helping you move from your hospital bed to a chair. By the second day, you'll begin walking longer distances using your crutches or walker.
You may not be allowed to put weight on the affected leg for a period of time. This varies from surgeon to surgeon and is also affected by how well your surgeon thinks the operation went.
Your physiotherapist will go over exercises to begin toning and strengthening the thigh and hip muscles. Ankle and knee movements are used to help pump swelling out of the leg and to prevent the formation of blood clots.
You will need to follow hip dislocation precautions--just like after your first artificial hip replacement. The risk of dislocation after a revision is higher than after a primary hip replacement.
Patients are usually able to go home after spending four to seven days in the hospital. You'll be on your way home when you can demonstrate a safe ability to get in and out of bed, walk up to 75 feet with your crutches or walker, go up and down stairs safely, and consistently remember to use your hip precautions. Patients who require extra care may be sent to a different unit until they are safe and ready to go home.
Most of the time your surgeon will see you one or more times during outpatient visits. Depending on what is learned from the examination and X-rays, you may start to put full weight on your leg. Because the operation is more complicated than primary replacement surgery and the period of walking on crutches may take longer, you must realize that it will take at least a year to be able to perform all normal daily activities. In some patients the possibilities are more limited than before. Be aware that a revision hip prosthesis is not as good as a primary prosthesis. There is always a chance that the donor bone will disappear in time because it is dead material and will be reabsorbed by the body. This means that loosening can occur once more. Today no other materials are available that are superior to donor bone.
Most orthopedic surgeons recommend that you have routine checkups after your revision surgery. How often you need to be seen varies from every six months to every five years, according to your situation and what your surgeon recommends. You should always consult your orthopedic surgeon if you begin to have pain in your artificial joint or if you begin to suspect something is not working correctly.
Portions of this document copyright MMG, LLC.